For those unfamiliar with what a Critical Access Hospital is or how it operates, this article breaks down what you need to know. We'll walk through the origins and function of CAHs, explain the impact of new federal legislation, and show how all of this is reshaping rural health care as we know it.
Whether you're part of a rural hospital, a local official, or someone simply concerned about access to care in rural communities, this piece will help you understand the stakes — and the urgent need for action.
What Is a Critical Access Hospital (CAH)?
Critical Access Hospitals (CAHs) are the backbone of rural health care in the United States. These small facilities provide emergency and inpatient services in remote areas where patient volume is low and travel to larger hospitals can be life-threatening.
Designated under a special Medicare status, CAHs are reimbursed based on their actual costs rather than fixed rates. This cost-based reimbursement helps them remain financially viable in regions that would otherwise be medically underserved.
Why CAHs Were Created
CAHs were established in 1997 through the Balanced Budget Act and the Medicare Rural Hospital Flexibility Program. They emerged as a response to a devastating wave of rural hospital closures in the 1980s and early 1990s. At the time, lawmakers envisioned CAHs as a temporary measure — a bridge until more sustainable models could be developed.
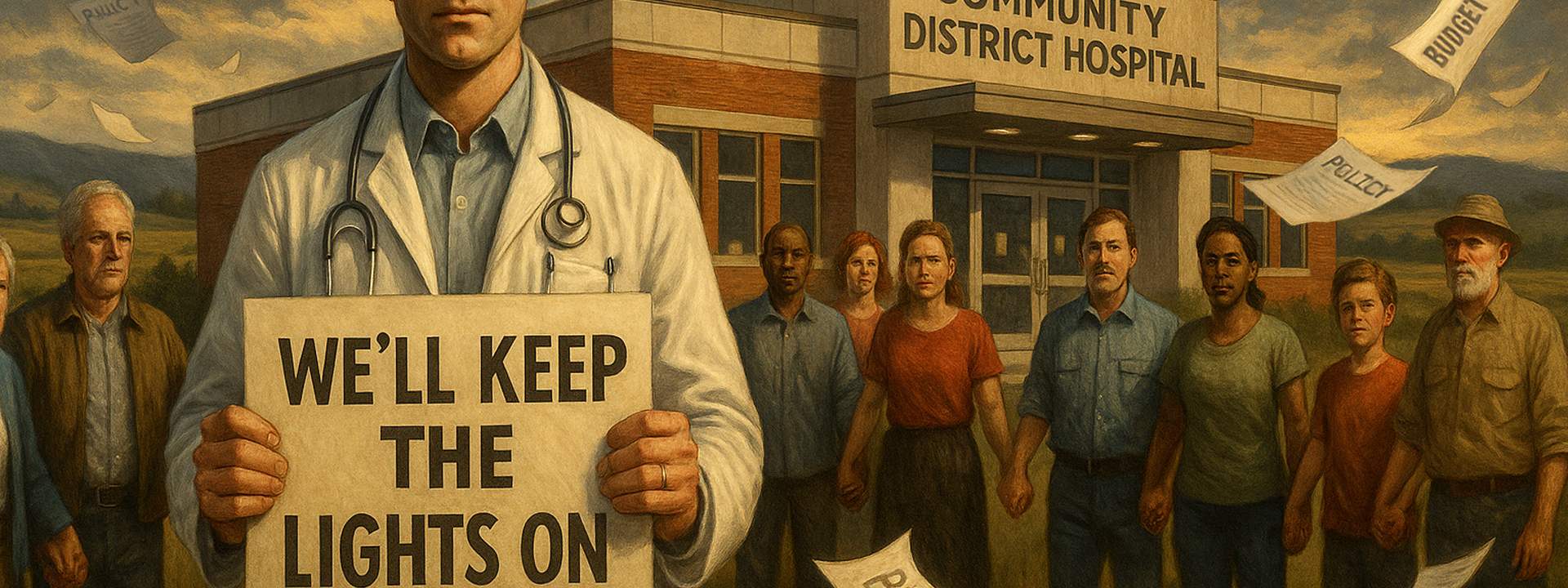
There was no expiration date written into the law. But the intent was clear: keep the lights on in rural hospitals while policymakers found long-term solutions.
Why CAHs Became Permanent
According to the University of North Carolina’s Cecil G. Sheps Center for Health Services Research, more than 140 rural hospitals have closed since 2010 — and most of them were not Critical Access Hospitals. This ongoing closure trend reinforces why CAHs have become a default financial survival mechanism for rural care.
That long-term solution never materialized.
Instead, CAHs have become a cornerstone of rural health policy for several reasons:
- Persistent rural health disparities
- Ongoing closures of non-CAH facilities
- Low patient volume and high operating costs in rural areas
- Lack of other systems to ensure 24/7 access to emergency and inpatient care
As of 2024, more than 1,350 CAHs operate across the U.S., serving approximately 20% of the rural population. In many regions, they are the only source of hospital care.
And in many small towns, the local hospital isn't just a health care provider — it's one of the key pillars of the local economy, alongside the school and the bank. When a hospital shuts down, the ripple effect is enormous: jobs are lost, residents move away, and the entire community begins to hollow out.
A New Option: The Rural Emergency Hospital (REH)
The Rural Emergency Hospital (REH) designation was officially created through the Consolidated Appropriations Act of 2021 and began accepting hospital conversions on January 1, 2023.
The REH concept draws heavily from what was known as the "Montana Model"—a rural health strategy piloted in the 2010s. In that model, some of Montana’s smallest hospitals dropped inpatient services but kept their emergency departments and outpatient clinics open. The approach helped stabilize finances and preserve essential services for extremely rural communities.
REH takes that same principle nationwide. It offers federal support, including monthly payments and enhanced Medicare reimbursements, to make the model financially viable in the long term.
In recognition of ongoing rural health care challenges, Congress created the Rural Emergency Hospital (REH) designation before the Big Beautiful Bill was introduced. This new status allows rural hospitals to convert voluntarily to a model that focuses on emergency, outpatient, and observation services only.
REHs forgo inpatient beds in exchange for a monthly facility payment and increased Medicare reimbursement rates. The model is designed to support facilities in areas where maintaining full inpatient services is no longer viable.
Though it offers flexibility and potential financial relief, REH status has been met with mixed reactions. Like CAHs when they were first introduced, REHs are often seen as a downgrade or "second-class" status. Some worry that converting to an REH means losing critical services or signaling decline.
But in the right setting — sparsely populated, geographically isolated areas where full-service hospitals struggle to survive — REH could be the right move. The concern now is that the rollout of REH came just before the passage of the Big Beautiful Bill, which may undercut its viability. The timing is unfortunate.
Enter the Big Beautiful Bill
The Budget Reconciliation and Tax Reform Act of 2025 — informally known as the "Big Beautiful Bill" (BBBA) — is reshaping the health care landscape in rural America. Though touted as a comprehensive budget and tax reform, the bill introduces sweeping Medicaid cuts that pose an existential threat to CAHs.
What's in the Bill?
1. Medicaid Cuts — Nearly $1 Trillion Over 10 Years
- Shifts funding to state block grants
- Introduces per-capita caps
- Adds eligibility barriers like work requirements and annual re-verifications
For CAHs, which rely heavily on Medicaid reimbursements, this is catastrophic. The average CAH receives around $3.9 million annually from Medicaid. That money is now uncertain.
2. Rural Hospital Relief Fund — $50 Billion Over 5 Years
- Meant to offset some of the damage
- If divided equally, CAHs might get ~$1M/year
Sounds helpful. But it covers only about 7% of the projected losses, according to the Center for Rural Strategies.
3. New Eligibility Requirements
- Starting in 2027, millions are expected to lose coverage
- Even eligible individuals may fall off Medicaid rolls due to stricter checks
This increases the number of uninsured patients showing up in rural ERs. That means higher uncompensated care costs, more strain on limited resources, and even higher odds of hospital closures.
Short-Term Impacts: What We're Already Seeing
- Some CAHs are cutting OB services and emergency care to stay solvent
- Layoffs and department closures are being planned in anticipation of revenue drops
- Facilities in Texas, Iowa, and Arizona are already sounding the alarm
Long-Term Outlook
Without intervention, the U.S. could see:
- A sharp rise in rural mortality
- Loss of emergency care access for millions
- Deepening of rural-urban health disparities
- Accelerated economic decline in rural communities
What started as a stopgap fix in 1997 has become an irreplaceable institution. And it's now being quietly dismantled.
For Leadership and Administrators
As Medicaid reimbursements dwindle, leadership in rural health care organizations will need to scrutinize their budgets. With less coming in, there must be less going out.
That means cutting costs in operational areas — especially in cost centers like IT. Strategic decisions made now will determine which rural hospitals survive the next five years.
But tightening the belt doesn’t mean compromising on quality. It means being smarter with the dollars we still have — prioritizing outcomes, investing wisely, and working with partners who understand the stakes and are committed to helping us do more with less.
Tech Debt Is Real — And Expensive
If you're trying to cut costs in IT, the last thing you want to do is end up with a mess that's more expensive to manage later.
Tech debt refers to the long-term cost of quick or poorly informed decisions — and in small health care environments, it often looks like this:
- 20 different vendors, each doing things their own way
- A network where nothing aligns with your internal standards
- IT staff constantly putting out fires instead of maintaining a clean, stable environment
It becomes a never-ending cycle of patching, fixing, reconfiguring — and it burns out your people while draining your budget.
One of the biggest causes? Medical software that gets purchased before IT is involved.
Whether it’s a clinical app or a major infrastructure system, throwing new software at IT after the contract is signed is asking for trouble. It’s how critical vulnerabilities and long-term inefficiencies sneak in.
Instead, organizations should adopt a formal application intake process — one that:
- Engages IT early in the selection process
- Triggers a HIPAA risk analysis before purchase
- Applies to all new applications and all major upgrades to existing systems
We've helped several hospitals implement this at visuaFUSION, and the impact is immediate. Less chaos. Fewer surprises. Better security. Better budgeting.
And here’s the part many don’t realize:
👉 It’s not your vendor’s job to secure your environment — it’s yours.
As an example, we’ve reviewed software from one of the biggest known vendors in medication dispensing, and found:
- End users required to remote into servers using shared administrator accounts
- User Account Control (UAC) and Windows Firewall disabled
- No client software available — so users interact directly with critical servers
- No support for automated patching
- Domain integration that involves actively disabling domain security policies
All of this — from a product that costs 40% more than alternatives.
That’s why we highlight solutions like 3AM Technologies. They focus on small health care organizations, and offer a medication dispensing platform that:
- Installs cleanly on workstations
- Runs securely without admin rights
- Doesn’t force security compromises
- Uses modular cabinet designs, so you can replace PCs without replacing the whole cabinet
- Is fully HL7 compliant (integrates with EHR/EMR)
- Costs ~40% less up front, and saves even more over time
Their solution is every bit as robust — without the added cost or risk. Like us, they’re built specifically for small health care environments. They understand your limitations and work with you, not against you.
If your organization is planning to implement or upgrade a medication dispensing platform, talk to 3AM before making any decisions. In many cases, switching is actually less expensive than upgrading, and you'll be setting your organization up for serious long-term savings. Their website: https://3amtechnologies.com/.
4 More Areas Where Most Small Hospitals Are Overspending
Medication dispensing isn’t the only area where rural health care orgs are paying too much for too little.
We regularly help CAHs and REHs identify savings in four other key categories:
- Email Providers — Are you overpaying for email? We’ve helped rural hospitals cut costs by thousands just by exploring condensing software vendors - utilizing programs and special licensing available for rural health care, orgs can save thousands per month in this area alone.
- Microsoft Licensing — Rural hospitals often qualify for special programs... and don’t even know it. In addition, vendor discounts separately and on top of those programs exist for small health care orgs.
- Email Encryption — Some vendors charge $4–6 per user/month — and then lock you into stripped-down versions with minimum seat counts.
- Phishing Simulation — You don’t need to pay $2-3000 per year to collect data on who your risky users are and train them against real threats. You need affordable, no-BS solutions that work.
We’ll break down all of these — with real savings data and examples — later on in this piece.
Because when every dollar matters, these aren’t small decisions. They’re survival strategies.
Regulatory Uncertainty: HIPAA and the Change Healthcare Breach
In February 2024, Change Healthcare — a UnitedHealth subsidiary — suffered one of the largest health care data breaches in history, affecting over 100 million individuals. The attack disrupted billing, claims, and patient care nationwide. While media coverage has waned, the regulatory ripple effects are still unfolding.
As of July 2025, no legislation has directly passed in response to the breach. But the U.S. Department of Health and Human Services (HHS) has proposed significant updates to the HIPAA Security Rule. These updates include stricter requirements for encryption, multi-factor authentication, annual audits, and faster patch cycles. CMS is also drafting rules that may make cybersecurity compliance a condition of participation in Medicare and Medicaid programs.
These changes present a serious compliance challenge — especially for small health care organizations like CAHs and REHs. Expect both labor costs (due to audits, risk assessments, vendor coordination) and capital costs (new equipment, encryption tools, patch management systems) to rise.
Now more than ever, it's important to work with vendors who help you meet new requirements without charging enterprise prices for essential services.
The Change Healthcare breach exposed just how vulnerable third-party vendors are. Small health care orgs need strategic partners who can help them navigate not only today’s budget crisis — but also tomorrow’s regulatory ones. Finding vendors who stand beside you, not above you, is essential.
Small organizations who care about each other’s survival are better off working together than begging for scraps alone. A partnership with visuaFUSION isn’t just another line item from a large vendor. You are not a footnote in our business — you are the foundation of it.
Final Thoughts on the Current State of Things
The Critical Access Hospital program was never meant to be permanent. But for many communities, it has become essential.
The Big Beautiful Bill's Medicaid cuts threaten to undo decades of rural health policy. And unless additional relief or policy corrections are made, CAHs across the country may be forced to shutter their doors.
The newly introduced Rural Emergency Hospital model offers a narrow path forward for some. But for most, it's arriving in the middle of a storm.
At visuaFUSION, we're not just vendors. We're allies.
We work exclusively with small health care organizations, including rural hospitals, long-term care, and critical access facilities. We know that if you survive, we survive. Rural health care matters — and we want to help you get through this.
Our Pledge to CAHs and REHs in 2025: A Free Year of Phishing Simulation
In response to this growing crisis, we're offering a full year of phishing simulation free to any Critical Access Hospital or Rural Emergency Hospital.
✅ No catch. No surprise costs. Just support for the folks who need it most.
This helps eliminate one line item from the budget while still protecting your users from one of the biggest threats in health care IT today. We're also typically half the cost or less on an ongoing basis when compared to other vendors commonly used for phish testing in small health care organizations- so this is not some trick up front to lock you into a higher cost product later - this is a smart move that will help eliminate a bill now and reduce a necessary expense considerably long-term.
Here’s how to get started:
- Sign up for a free trial: https://phishingsim.visuafusion.com
- Validate your domain and watch the walkthrough: https://visuafusion.com/ClientPortal/Docs/PhishingSim
- Schedule a short validation call: https://api.leadconnectorhq.com/widget/bookings/phishingsim-freeyearoffer
We’ll confirm your CAH or REH status and activate your free Basic Plan for one year.
We Align With You — Not Against You — And Help You Stretch Every Dollar
These aren't just one-time budget wins — they're recurring, long-term savings strategies that help stabilize IT spend year after year.
✅ Warrantied Windows 11-Ready PCs Starting at $324 Skip the $800–$1400 new hardware price tags. We offer Lenovo enterprise-class machines that are fully tested, warrantied, and ready for Windows 11 — all at a fraction of the cost. View our hardware options
✅ Managed Firewall & Network Solutions Our enterprise-class security and connectivity solutions often come in at half the cost of competitors. If you're working with limited budgets and high compliance expectations, let’s talk. Contact us
We understand the realities of small health care budgets. And our business is built around supporting you — not squeezing you.
✅ Full outbound email encryption for just $3.20/user/month Where others charge $4–6 for stripped-down, basic plans with minimums and limitations, we deliver full-featured encryption with no gimmicks and no tiered trickery. This alone typically saves small health care organizations thousands per year. Learn more
✅ Backup software priced for small health care We provide enterprise-grade, scalable backup and disaster recovery through Quest Rapid Recovery — at massive discounts for small providers. Details here
✅ Microsoft licensing guidance + discounts If you're a rural hospital currently using Google for email, you could be leaving thousands in savings on the table. We help you qualify for Microsoft’s Rural Hospital Program, and go further by adding our own discounts on top. This alone typically saves small health care organizations thousands per year. Explore licensing help
Need a More Hands-Off, Fully Managed Option?
(Recurring strategic savings opportunity)
For organizations that feel overwhelmed by the complexity of health care IT — or simply want to join a model that's already built and maintained — we also offer visuaFUSION HealthNet.
HealthNet is a professionally managed, shared health care IT environment built specifically for small providers. It removes barriers, ensures compliance, and delivers enterprise-grade IT performance without the enterprise-grade price tag.
✅ Enterprise infrastructure, shared and scalable ✅ Deeply discounted through cooperative cost-sharing ✅ Includes full IT policies, systems management, networking, backups, and support ✅ A team of IT professionals covering various IT specialties maintaining the environment ✅ You keep your local IT for hands-on help — we take care of the rest.
With HealthNet, you get the structure, support, and security of a large health system — while staying independent. Learn more
Overall, there are options out there and leaders in rural health care will need to get creative, as they always have, in order to weather the storm. Know that we see you out there fighting to keep the lights on for your communities, and that you are not alone. Keep pushing. Let’s get through this together.
Sources & Citations
- UNC Cecil G. Sheps Center for Health Services Research 140+ Rural Hospital Closures Since 2010
- Kaiser Family Foundation (KFF) Medicaid spending and policy impact estimates https://www.kff.org
- Center for Rural Strategies Commentary on the BBBA's limited relief funding vs projected losses https://www.ruralstrategies.org
- Cronkite News / Arizona PBS Reporting on anticipated cuts to OB and ER services at Arizona CAHs
- Houston Chronicle Editorial coverage on Texas rural health and BBBA impact
- Associated Press (AP) Analysis of expected CAH closures and financial strain post-BBBA
- U.S. Department of Health and Human Services (HHS) HIPAA Security Rule Proposed Rulemaking (January 2025) https://www.hhs.gov/hipaa
- Healthcare Sector Cybersecurity Performance Goals Released by HHS in January 2024 in response to national vulnerabilities
- Senate Hearings, May 2024 Congressional review of the Change Healthcare breach and calls for stronger vendor oversight
- Change Healthcare Cyberattack Overview Widely reported breach affecting 100M+ individuals — February 2024
- CMS Office of Enterprise Data and Analytics Signaling future regulatory link between cybersecurity and Medicare/Medicaid participation
- Log in to post comments